PHYSIOLOGY OF PLEURAL FLUID PRODUCTION AND BENIGN PLEURAL EFFUSION.
PHYSIOLOGY OF PLEURAL FLUID PRODUCTION AND BENIGN PLEURAL EFFUSION. Pleural Effusion . More than 1 million case of pleural effusion occurred annually in US.
Share Presentation
Embed Code
Link
Download Presentation
- immunohistochemical test
- pleural effusion resolve
- hemoptysis
- insufflate talc
- lung interstitium
- cardiac injury

paulina + Follow
Download Presentation
PHYSIOLOGY OF PLEURAL FLUID PRODUCTION AND BENIGN PLEURAL EFFUSION.
An Image/Link below is provided (as is) to download presentation Download Policy: Content on the Website is provided to you AS IS for your information and personal use and may not be sold / licensed / shared on other websites without getting consent from its author. Content is provided to you AS IS for your information and personal use only. Download presentation by click this link. While downloading, if for some reason you are not able to download a presentation, the publisher may have deleted the file from their server. During download, if you can't get a presentation, the file might be deleted by the publisher.
Presentation Transcript
- PHYSIOLOGY OF PLEURAL FLUID PRODUCTION AND BENIGN PLEURAL EFFUSION.
- Pleural Effusion • More than 1 million case of pleural effusion occurred annually in US. • On lateral decubitus chest radiography, the distance between inside of chest wall and out side of lung is greater than 10 mm, diagnostic thoracentesis is indicated.
- FORMATION AND RESORPTION OF PLEURAL EFFUSION. • Pleural effusion have several origins--- 1).Capillary in parietal and visceral pleura. 2).Interstitial space of lung. 3).Peritoneal cavity--- Through small hole in diaphragm. • Rate entry into the pleural space in normal-- 0.01 ml/kg per hour.
- Fig. 57-1.
- Pleural Effusion • Capillary origin--- Starling law of transcapillary exchange: Qf=Lp x A【(Pcap-Ppl)-σd(πcap-πpl)】. • Interstitial origin---exudate , increased permeability, pulmonary edema also originate from lung interstitium. • Peritoneal origin--- Cirrhosis and ascites, pancreatic ascites, Meigs’ syndrome, peritoneal dialysis.
- Pleural Effusion • Lymphatic clearance--- the lack of fluid accumulation in pleural cavity normally. • The pleural space--- communication with lymphatic vessels by stomas located in parietal pleura., removed the protein, cell, particle matter. • Clearance rate--- 0.2-0.28 ml/kg per hour. • Lymphatic clearance--- 28 times as high as the normal rate of pleural fluid formation.
- DIFFERENTIAL DIAGNOSIS Table 57-1
- DIFFERENTIAL DIAGNOSIS • Transudate--- Increase hydrostatic pressure or decrease oncotic pressure. • Exudates--- Increase permeability. • Three criteria--- The exudates meet at least one, the transudate meet none : 1) pleural fluid protein/ serum protein > 0.5 2) pleural fluid LDH/ serum LDH > 0.6. 3) pleural fluid LDH > 2/3 upper normal limit for serum LDH.
- DIFFERENTIAL DIAGNOSIS • The difference between the serum and pleural fluid albumin exceeds 1.2--- Transudate. • Pneumonia, malignancy, pulmonary embolism account the great majority of all exudates. • Undiagnosed exudates : Check glucose level, amylase, LDH, diffrential cell count, microbiological studies, cytoloty, pH, adenosine deaminase(ADA), interferon-γ, polymerase chain reaction(PCR)for tuberculosis DNA, lipid analysis. • Gross appearance of pleural effusion and odor. • Hematocrit over 50%--- Hemothorax.
- Pleural fluid--- WBC count and differential • Greater than 10000 per μL--- Parapneumonic effusion, pancreatitis, pulmonary embolism, collagen vascular disease, malignancy, tuberculosis. • Polymorphonuclear(PMN) leukocytosis--- Acute disease such as pneumonia, pulmonary embolism, pancreatitis, intra-abdomen abscess, early tuberculosis. • Mononuclear cell--- Malignancy, tuberculosis, resolving acute process. • Eosinophil--- Benign asbestos, drug reaction as nitrofurantoin, bromocriptine, dantrolene, paragonimiasis(low glucose, low pH, high LDH). • More than 50% WBC in exudates are small lymphocyte--- malignancy or tuberculosis.
- Pleural fluid--- glucose • Less than 60 mg/dL--- parapneumonic effusion or empyema, malignant effusion, tuberculosis effusion, rheumatoid effusion(usually less than 30), hemothorax, paragonimiasis effusion, Churg-Strauss syndrome. • Less than 40 mg/dL--- Tube thoracostomy should be performed.
- Pleural fluid--- amylase • Elevated above the upper normal limit of serum amylase---- Esophageal perforation(from salivary), pancreatic disease, malignancy(10%). • Acute pancreatitis accompanying pleural effusion--- 10%. • Chronic pancreatic disease may develop a sinus tract between the pancrease and the pleura space. • The amylase associated with malignancy--- salivary type.
- Pleural fluid--- lactic acid dehydrogenase • Pleural fluid lactic acid dehydrogenase---good indicator of the degree of inflammation in pleural space. • LDH increase, the inflammation worsening.
- Pleural fluid--- cytology • Establishing the diagnosis of malignant pleural effusion--- 40-90%. • Depending on--- the tumor type, amount of fluid, skill of cytologist. • Cytology result usually positive if the primary tumor is adnocarcinoma, usually not positive if the primary tumor is squamous cell carcinoma, lymphoma, mesothelioma. • Immunohistochemical test using monoclonal antibody--- differentiate adenocarcnoma, benign mesothelial and malignant methelial cell.
- Pleural effusion--- bacteriology • Culture and bateriologic stain--- culture both aeobic and anaerobic, mycobacteria, fungi. • Gram’s stain.
- Pleural fluid--- pH and pCO2 • Less than 7--- Complicated parapneumonic effusion and tube thoracostomy should instituted. • Less than 7.2--- systemic acidosis, esophageal rupture, rheumatoid pleuritis, tuberculosis pleuritis, malignant pleural disease, hemothorax, paragonimiasis, Churg-Strauss syndrome.
- Diagnosis of tuberculous pleuritis • ADA level, interferon-γ, PCR for tuberculosis DNA. • ADA level above 47 U/L, combined with pleural fluid lymphocyte/ neutrophil > 0.75(no commercial ) . • Interferon-γlevel > 3.7 U/ml.
- Pleural fluid • Other diagnostic test on pleural fluid--- cloudy. • Chylothorax---Triglycerides > 110 mg/dl, • Pseudochylothorax--- the level of cholesterol increase.
- INVASIVE TEST FOR UNDIAGNOSED EXUDATIVE PLEURAL EFFUSIONS • 20% exudates--- no diagnosis. • Needle biopsy. • Thoracoscopy. • Bronchoscopy. • Open biopsy of the lung.
- Needle biopsy of pleura • For diagnosis of Tuberculous pleuritis, malignant pleural disease. • The needle biopsy usually negative when negative cytology result.
- Thoracoscopy • Direct visualized. • Became primary means of diagnosing pleural malignancy who have negative cytology result(95%). • Insufflate talc at the time of thoracoscopy. • Video-Assisted Thoracoscopic Surgery. (VATS).
- Bronchoscopy • Not all need. • Only used at patient with 1) parenchyma abnormality. 2) Hemoptysis.
- Open biopsy of the lung • Provide the best biopsy specimens. • Has been replaced by VATS.
- TRANSUDATIVE PLEURAL EFFUSIONS. • Hepatic hydrothorax. • Nephritic syndrome. • Congestive heart failure. • Peritoneal dialysis.
- Congestive heart failure • Bilateral, same size on each side. • Left ventricular or bi-ventricular failure. • Can be observed while the heart failure is treated and usually resolves. • Pleurodesis with sclerosing agent only if persistent pleural effusion despite intensive therapy of heart failure.
- Hepatic hydrothorax • 5%, direct movement of peritoneal fluid through small hole in diaphragm. • Usually right side, large. • Treatment--- reverse the liver disease, liver transplant, implantation of transjugular intrahepatic portal systemic shunt. Peritoneal jugular shunt. • Pleurodesis is contraindicated--- danger of hypovolemia.
- Hepatic hydrothorax • Spontaneous bacterial empyema--- infection of hepatic hydrothorax. • 13%. • Diagnosis criteria--- 1). Positive pleural fluid culture. 2). Pleural fluid neutrophil greater than 250 cells/mL. Treatment--- tube thoracostomy.
- Nephritic syndrome • Decrease plasma oncotic pressure. • 20%. • Treatment--- increase level of serum protein.
- Peritoneal dialysis • Diaphragm defect. • Treatment--- 1). Chemical pleurodesis. 2). Short period of small-volume, intermittent peritoneal dialysis.
- EXUDATIVE PLEURAL EFFUSIONS • Pulmonary embolization. • Esophageal perforation. • Acute pancreatitis. • Chronic pancreatic disease. • Intra-abdominal abscess.
- Pulmonary embolization • S/s--- dyspnea. • Less than 1/3 of hemithorax, bilateral. • Bloody or clear. • Neutrophil mostly, lymphocyte or mononuclear. • Dx--- lung scan, contrast-enhanced spiral CT, pulmonary arteriography. • Tx--- same with pulmonary emboli.
- Esophageal perforation • Mortality 100% if not diagnosis in 48 hours. • S/s--- Acutely ill with chest pain, dyspnea, mediastinal and pleural effusion, subcutaneous emphysema. • Dx--- Level of amylase of pleural fluid, contrast studies. • Tx--- Exploration of mediastinum and primary repair esophageal tear, drainage, antibiotics, T-tube intubation.
- Acute pancreatitis • 50%, bilateral most. • S/s--- pleural chest pain, dyspnea. • Pancreatic pseudocyst--- high in pleural effusion. • Pleural effusion not resolve in 2 week---pancreatic abscess or pseudocyst is considered.
- Chronic pancreatic disease. • Sinus tract through diaphragm into mediastinum and pleural cavity. • S/s--- chest pain, dyspnea, cough. Most without abdominal sign. • Left side, recurs rapidly after thoracentasis. • Dx--- high amylase in pleural effusion, ERCP. • Tx--- first 2-3 week conservative treatment, (NG tube, NPO, atropin, repeat thoracentasis, continuous infusion somatostatin), failure then laparotomy, (ligated and excised sinus tract, partial pancreatectomy, Roux-en-Y loop.)
- Intra-abdominal abscess • Subphrenic, pancreatic, intrasplenic, intrahepaic. • Dx--- pleural fluid predominantly neutrophil, CT, antibiotics and drainage.
- PLEURAL EFFUSION AFTER SURGICAL PROCEDURE • After cardiac injury. • After CABG. • After Fontan procedure. • After abdominal surgery. • After endoscopic variceal sclerotherapy. • After liver transplantation. • After lung transplantation.
- After cardiac injury • Postcardiac injury syndrome(Dressler’s syndrome)--- pericarditis, pleuritis, pneumonitis. • 3 week after injury(3 day-1 year). • Exudates, clear or bloody. • Tx--- anti-inflammatory agents(aspirin, indomethacin,). Corticosteroid for CABG--- prevent pericarditis and graft occlusion.
- After CABG • Small pleural effusion, high prevalence,(40%.) • Pathogenesis--- unknown, may pericardial inflammation. • Left side, resolve spontaneously.
- After CABG • Some massive pleural effusion, no clear-cut etiology. • Exudative. • Bloody--- Related to blood from surgery. Maximal size in 30 day, peripheral eosinophilia, high fluid LDH, responded with thoracenteses. • Non-bloody--- More than 30 days, more than 50% small lymphocyte, low LDH, more difficult mamage, require pleurodesis,
- After Fontan procedure • Fontan procedure--- right ventricle is bypassed by an anastomosis between superior vena cava, the right atrium, inferior vena cava and the pulmonary artery. • Usually performed for tricuspid atresia or univentricular heart. • Transudate pleural effusion. • Occurred in all patient, most occurred in patient with significant aortopulmonary collateral vessels preoperatively.. • Tx--- inserting pleuroperitoneal shunt, creation of a late fenestration.
- After abdominal surgery • 50%, 2-3 day after operation. • High incidence in upper abdomen surgery, postoperative atelectasis, free abdominal fluid at surgery. • Cause--- diaphragm irritation trans-diaphragm movement of intra-abdomen fluid. • Thoracenteses--- R/O pleural infection. • More than 72 hours post operatively, not related to surgical procedure, may due to pulmonary embolism, intra-abdominal abscess, hypervolemia.
- After endoscopic variceal sclerotherapy • 50%. • Extravasation of sclerosant into esophageal mucosa, intense inflammatory reaction. • Exudative. • Persist 24-48 hours, accompanied by fever. • Tx--- thoracentesis.
- After liver transplantation • Right side, within 72 hr. • Large enough for respiratory compromised, • Tube thoracostomy. • Etiology unknown, may irritation the right hemidiaphragm by extent right upper quadrant dissection and retraction. • Prevent by fibrin sealant.
- After lung transplantation • Fluid leave lung via lymphatics exits into pleural space. • 400 ml/day, up to 1000 ml. • Chest tube drainage.
- Rheumatoid • Glucose--- less than 30 mg/dl. • High LDH--- 700IU/l. • Low pH--- less than 7.2. • Resolves spontaneously within 3 months.
- Lupus erythematosus • 40%. • Tx--- Prednisolone, 80 mg/day.
- Asbestos exposure • 3%. • Need exudates 5-20 years. • Always asymptomatic. • Dx: exposure, exclusion other cause. • Follow up at least 2 year.
- Drug reaction • Nitrofurantoin Dantrolene Methysergide Bromocriptine • Tx--- discontnuation the drug.
- Uremia • 3%. • Exudates. • No relationship between degree of uremia and occurrence of pleural effusion. • Disappear within 4-6 week after dialysis.
Pleural Effusion
Pleural Effusion. Accumulation of fluid within the visceral and parietal layers of the pleura when there is an imbalance between formation and absorption in various disease states.
2.86k views • 42 slides
PLEURAL EFFUSION
PLEURAL EFFUSION. 2. 1. Right pleural effusion blunting the right costophrenic angle extending posteriorly with some fluid tracking into the major fissure seen on the lateral exam. Upright. 3.
1.4k views • 23 slides
Pleural effusion
7/1/2012. 2. Causes of Pleural Effusion Transudates increase venous pressure (cardiac failure, constrictive pericarditis, fluid overload) hypoproteinaemia (cirrhosis, nephrotic syndrome, malabsorption) hypothyroidism Meig's syndrome (due to a benign ovarian tumor) . 7/1/2012. 3. Causes of
1.03k views • 32 slides
TB pleural effusion
TB pleural effusion. 林倬睿醫師. Outlines . Introduction Etiology & pathogenesis Symptoms, laboratory & radiologic findings Diagnosis Treatment & management Complications . Introduction . 是由結核菌感染肋膜所引起 通常為 exudate, 可以同時合併肺部病灶 為最常見的肺外結核表現
1.89k views • 35 slides
Pleural effusion
Definition:. A pleural effusion is an excessive accumulation of fluid in the pleural space. It can be detected on X-ray when 300 ml or more of fluid is present and clinically when 500 ml or more is present. The chest X-ray appearances range from the obliteration of the costo-phrenic angle to dense
1.02k views • 28 slides
Pleural Effusion
Pleural Effusion. GenMed 3. Development of Pleural Effusion. pulmonary capillary pressure (CHF) capillary permeability (Pneumonia) intrapleural pressure (atelectasis) plasma oncotic pressure (hypoalbuminemia) pleural membrane permeability (malignancy)
977 views • 13 slides
Malignant Pleural Effusion M.P.E.
Malignant Pleural Effusion (M.P.E.). .
669 views • 45 slides
Tuberculous Pleural Effusion
786 views • 13 slides
Pleural effusion
. Definition:A pleural effusion is an excessive accumulation of fluid in the pleural space. It can be detected on X-ray when 300 mL or more of fluid is present and clinically when 500 mL or more is present. The chest X-ray appearances range from the obliteration of the costophrenic angle to dense
7.36k views • 28 slides
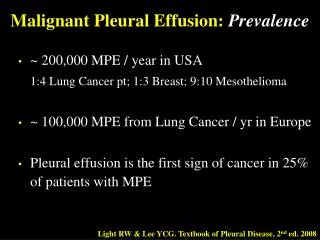
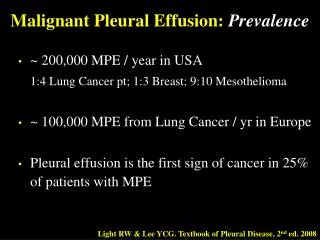
Malignant Pleural Effusion: Prevalence
Malignant Pleural Effusion: Prevalence. ~ 200,000 MPE / year in USA 1:4 Lung Cancer pt; 1:3 Breast; 9:10 Mesothelioma ~ 100,000 MPE from Lung Cancer / yr in Europe Pleural effusion is the first sign of cancer in 25% of patients with MPE.
1.52k views • 72 slides

Approach to Pleural Effusion
Approach to Pleural Effusion. Dr Abdalla Elfateh Ibrahim Consultant & Assisstant Professor of Pulmonary Medicine King Saud University . Definition Anatomy of the pleura Etiology & Pathophysiology Types of pleural effusions Clinical features
1.96k views • 49 slides
pleural Fluid Analysis
pleural Fluid Analysis. ll - pleural fluid analysis It comprises of pleural fluid appearance - Biochemical tests ( Protein, LDH). Cytological tests ( malignant cells, differential cell count) Microbiological tests ( Gram stain , AFB and culture). - PH analysis. Appearance ;
1.02k views • 21 slides
Pleural Effusion
Pleural Effusion. Group 2 B1 David, Hannah Lea David, Hazel Ann De Guzman, Jan Kristoper De Guzman, Raquel Isabelle De Leon, Gemma Rosa De Mesa, Angelica Monique. General Data. MP 61 /M Married From 1 Ma. Clara St. Quezon City Driver Roman Catholic Grade 3. Chief Complaint.
485 views • 15 slides
Pleural Effusion and +PPD
Pleural Effusion and +PPD. Sandy Valmadrid, MD 13 December 2006. Case. EH, 56 yo nonsmoker Shortness of breath, fever, night sweats Dc’d 3 days ago, St. Mary’s Hospital 102 fever, sob, cough WBC 19.3, neutrophilic predominance Cxray: RLL pneumonia Sputum: Streptococcus pneumoniae
442 views • 22 slides
Approach to Pleural Effusion
Approach to Pleural Effusion. Dr Abdalla Elfateh Ibrahim King Saud University. Pleural Effusion. Pleural effusions are a common medical problem with more than 50 recognized causes including disease local to the pleura or underlying lung, systemic conditions, organ dysfunction and drugs
1.07k views • 48 slides
TRANSUDATIVE PLEURAL EFFUSION
TRANSUDATIVE PLEURAL EFFUSION. Dr.Naresh Kumar Junior Resident Dept. of Pulmonary Medicine. TYPES OF PLEURAL EFFUSION. 1 EXUDATIVE 2 TRANSUDATIVE. TRANSUDATIVE PLEURAL EFFUSION.
1.69k views • 46 slides

Approach to Pleural Effusion
Approach to Pleural Effusion. Dr Abdalla Elfateh Ibrahim Consultant & Assisstant Professor of Pulmonary Medicine King Saud University. Pleural effusions. Abnormal collection of fluid in the pleural space resulting from excess fluid production or decreased absorption.
1.55k views • 48 slides

Approach to Pleural Effusion
Approach to Pleural Effusion. Dr Abdalla Elfateh Ibrahim Consultant & Assisstant Professor of Pulmonary Medicine King Saud University. Pleural Effusion. Pleural effusions are a common medical problem with more than 50 recognized causes including Local pleura disease
1.94k views • 48 slides
Pleural Effusion
Pleural Effusion. Larissa Bornikova, MD July 17, 2006. Objectives. To review the etiology and basic pathophysiology concepts related to pleural effusion. To understand indications for thoracentesis. To outline a systematic approach to diagnosing a cause of effusion.
1.07k views • 19 slides
Pleural effusion
Pleural effusion. Riahi taghi,M.D. Etiology. Fluid formation: parietal pleura Fluid removal: parietal pleura (lymphatic) Also enter from visceral pleura and diaphragm. Effusion finding. Blunting of costophrenic angle in CXR Sub pulmonic effusion White lung Phantom tumor Sonography
538 views • 19 slides